
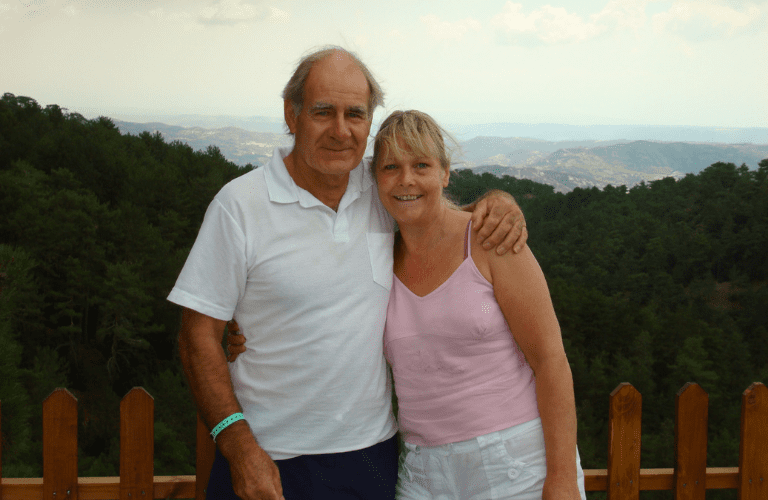
Tracy’s story
Tracy's husband Steve has Lewy body dementia, Tracy talks about support they've received from Admiral Nurse Liz.
Lewy body dementia is a progressive, complex and challenging condition which is thought to account for 10- 15% of all those with dementia. Around 10% of younger people with dementia have dementia with Lewy bodies. In the early stages it is often mistaken for Alzheimer’s disease and can be diagnosed wrongly.
Lewy body dementia includes two subtypes; dementia with Lewy bodies and Parkinson’s. It particularly affects the person’s ability to think and move and can cause hallucinations, fluctuations in alertness and sleep disturbances which can be extremely distressing for the person and their family.
The main difference between the two types of Lewy body dementia is when certain symptoms first occur:
As the condition progresses both people with dementia with Lewy bodies and Parkinson’s dementia tend to have similar symptoms and will have increasing difficulty with managing everyday tasks.
Lewy body dementia is caused by abnormal clumps of protein (called Lewy bodies) gathering inside brain cells. These Lewy bodies can build up in many parts of the brain but particularly in the areas responsible for thought, movement, visual perception and regulating sleep and alertness.
A person with Lewy body dementia might:
Memory is often less affected than with other types of dementia but people may be at more risk of mood and behaviour changes such as apathy, anxiety, depression, delusions and paranoia. One type of delusion, known as Capgras syndrome, in which the person believes that a friend or relation has been replaced by an imposter can be particularly difficult for families. Other symptoms may include changes in blood pressure, body temperature and impaired sense of smell.
It is important for someone with Lewy body dementia to get an accurate diagnosis so they get the right treatment and support. Diagnosis should include gathering information on the person’s symptoms and a specific scan called a SPECT (single photon emission computed tomography) scan may help support a diagnosis of Lewy body dementia.
People with Lewy body dementia may be offered medication and other interventions to help with their symptoms. These will not stop or reverse the course of the disease but can improve the quality of life for them and their families and carers.
Some of the medications used to treat Alzheimer’s disease can help with the cognitive symptoms of Lewy body dementia and can help reduce distressing hallucinations, concentration and memory problems. These are usually most effective in early or moderate phases but do not help everyone.
Importantly many people with Lewy body dementia are particularly sensitive to medications used to treat hallucinations and only certain types should be used with extreme caution.
Medications used for Parkinson symptoms may be helpful but again caution is required as they may make hallucinations worse.
Other interventions focus on symptom control and include; physiotherapy, occupational therapy, counselling, groups, cognitive stimulation therapy, music and activities.
For more information visit lewybody.org. You can also phone our free Dementia Helpline to speak to a dementia specialist Admiral Nurse about Lewy body dementia on 0800 888 6678 (Monday-Friday 9am-9pm, Saturday and Sunday 9am-5pm), email helpline@dementiauk.org or if you can pre-book an appointment by phone or video call with an Admiral Nurse.
Our virtual clinics give you the chance to discuss any questions or concerns with a dementia specialist Admiral Nurse by phone or video call, at a time that suits you.

Tracy's husband Steve has Lewy body dementia, Tracy talks about support they've received from Admiral Nurse Liz.

Rob's shares his story of partner Jayne, who experienced behavioural changes after a car accident and was diagnosed with dementia at the age of 59.
Julie writes about how her Admiral Nurse Rachel helped her understand the complexities of the health and social system – and her husband's diagnosis - when no one else could.