
I can’t imagine having more empathetic bosses
Glenn shares how flexible working arrangements and support from his managers enables him to continue working whilst prioritising his wife Helen's care.
Dementia can affect a person’s ability to manage their emotions and actions. At times of intense distress, they may become verbally or physically aggressive, putting them and those around them at risk of harm.
Factors that may lead to aggressive behaviour include:
Learning to assess factors that may put you or the person with dementia at risk is an important skill. It is helpful to follow these steps:
1. Try to identify what causes the person distress. For example, are they prone to sundowning?
2. Consider who this might put at risk. This could be the person with dementia themselves, you, or other people around them.
3. Make a plan to reduce the risk. For example, to help prevent sundowning, you could close the curtains before dusk to ease the transition from day to night.
4. Put these changes in place. If necessary, seek help from others, such as other family members or the person’s GP or social worker.
5. Keep reassessing the risk. Reflect on any changes – for example, a new carer or a change in the person’s dementia symptoms.
It is a good idea to put together a personal safety plan to use in situations where you feel at risk from the person with dementia.
Occasionally, the reactions of a person with dementia can tip over into domestic abuse or violence. This can be very difficult to talk about, but it is essential to get help, for example from the Admiral Nurse Dementia Helpline, your GP or domestic violence charities. Your local authority Adult Social Services Safeguarding Team can also offer support.
If you or anyone else feel at immediate risk, please call 999.
If you need advice on any aspect of dementia, please call the Dementia Helpline on 0800 888 6678 (Monday-Friday 9am-9pm, Saturday and Sunday 9am-5pm, every day except 25th December), email helpline@dementiauk.org or you can also book a phone or virtual appointment with an Admiral Nurse.
Our free, confidential Dementia Helpline is staffed by our dementia specialist Admiral Nurses who provide information, advice and support with any aspect of dementia.

Glenn shares how flexible working arrangements and support from his managers enables him to continue working whilst prioritising his wife Helen's care.

Will shares how his mum's diagnosis impacted the family and highlights the importance of advocating for young carers.
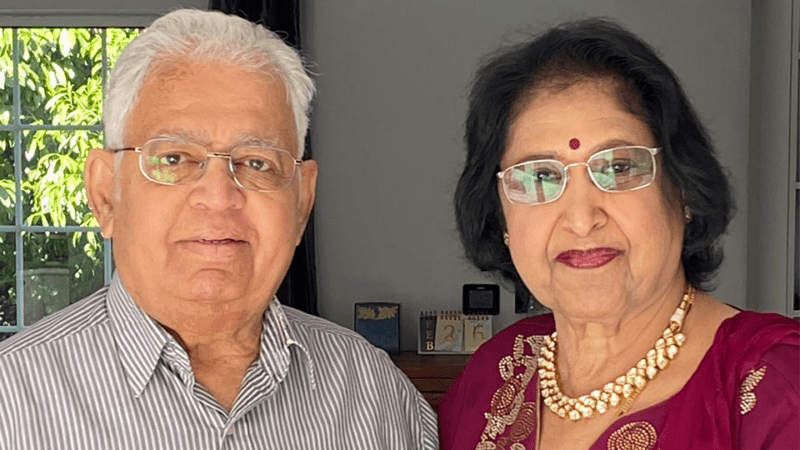
Pratibha shares her experience of caring for her late husband, Narayan Gopala, who lived with vascular dementia and died in 2024.