
Young onset dementia
Information and resources about young onset dementia, where symptoms develop before the age of 65.
When Pamela applied for NHS continuing healthcare for her husband Rob, she felt the odds were stacked against them from the outset.
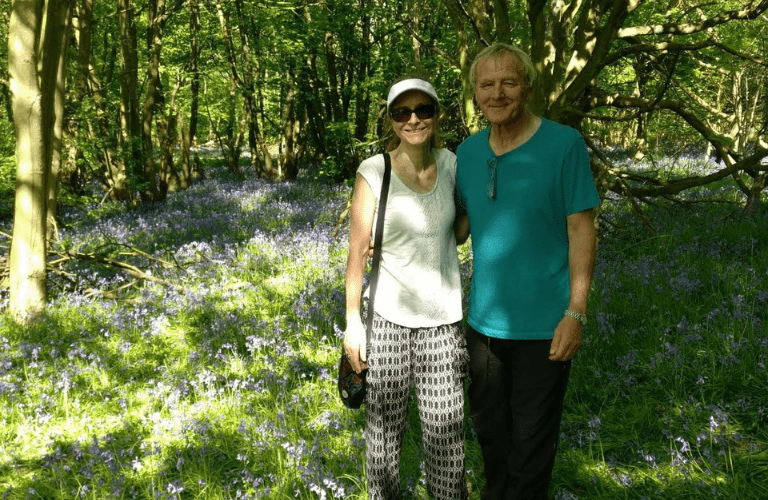
Rob and Pamela in Bluebell wood, May 2018
When my husband, Rob, was diagnosed with young onset Alzheimer’s disease at the age of 65, I thought we’d be able to get the support we needed – no one told me that I’d have a battle on my hands. When we applied for NHS continuing healthcare (CHC), a package of care fully paid for by the NHS, the odds were stacked against us from the outset.
It was heartbreaking to see the proud husband and father of our daughter and son, who were aged 20 and 18 at the time, become too disorientated to be looked after at home. He would try to hurt himself with knives and he’d leave to go home to his mum’s house, who died many years ago. He thought he was living with strangers in a strange house, and would search for anything familiar; and he only ever slept for a few hours at a time.
I had reduced my working hours and enlisted the help of family, but I knew we couldn’t go on like this.
It was then that the CHC funding was first mentioned. After an initial application for funding, raised by the Occupational Therapist, was ignored, I was advised by the Psychiatrist Consultant to get Robert into a home and the funding would be sorted out afterwards. It was vital to get him somewhere we were ‘happy with’ quickly to keep him and us safe. Rob was moved into a local nursing home, funded by his redundancy money, in February 2019.
After he escaped over the fence and was found almost a mile away as well as having a few altercations with other residents and care home staff, he was placed under round-the-clock care. When the home could no longer meet Robert’s complex needs, they gave me one month’s notice. He had been there less than 2 months.
Not only did I face £2,800 per week of 1-2-1 care costs to keep him in the home during the notice period, but Robert’s situation became increasingly uncertain. The redundancy money was quickly drained and I started to look elsewhere for a home specialising in young onset dementia.
The homes I tried all said he needed CHC funding to access their services – it wasn’t even an option for me to pay for his care. I was desperate at this point. We had to get CHC funding before anything could improve.
In March 2019, the CHC process was initiated by the lead nurse working in the care home who wanted to protect her staff and for Robert to get the most appropriate support. Robert’s case was also supported by our local MP who happened to be an ex-social worker with knowledge of the social care system and with access to the CHC Lead in the local area.
The first multi-disciplinary team assessment for CHC was convened with no social worker, psychiatrist or anyone with clinical knowledge of Robert’s dementia in attendance. Given Rob’s age and the fact that his dementia had progressed rapidly, I needed someone to understand that dementia can affect younger people differently. He was physically fit, healthy, and very strong but with no capacity to understand the world around him and had very little speech at this point.

Rob in 1993
From the minute I walked into that room, I was told that he was unlikely to get CHC, but I would be able to appeal. It was as if there was a brief not to give it to him.
A month later, the formal rejection was delivered, which was riddled with inaccuracies. I felt they’d got the wrong person; Robert’s age was wrong; it said that he had been in hospital when he hadn’t; it said he had declined to take part in the process when he had never been asked, or had capacity to even understand the question! Faced with a lengthy appeal process of three months, with no prospect of funding during that time, I made a complaint.

Rob and Pamela, February 2018
If you’re on your own, you have no chance. You’re exhausted, mentally and physically, and are rejected at every hurdle. It just seemed like professionals who were meant to support the system were always busy and under-staffed.
Emotional support at this time was provided by my Admiral Nurse. This support contrasted sharply to what we had experienced from the CHC panel. She was able to add notes to support Robert’s case. Her knowledge around the system and the deterioration brought on by the illness was invaluable when I couldn’t get to see a consultant. She was there for me. She visited us every fortnight whilst Robert was at home and was a constant source of support.
CHC was finally awarded, which allowed Robert to move into a specialist home in September 2019. It made a huge difference. The staff knew how to communicate with him and he settled really quickly. I was able to spend more time with him instead of fighting for appropriate support.
Rob in August 2018
It will always remain the most stressful time in my life. The toll it took on our children and myself cannot be underestimated.
Throughout the CHC process, the amount of time spent keeping records, writing reports, trying to get calls answered, attending meetings was time that could have been better spent with my husband. This was unforgiveable. Robert passed away in March 2021.
It is vital, we now come together to correct this unfair practice. This is why I’m supporting Dementia UK’s campaign to guide the way to a fairer and more consistent CHC process.

Information and resources about young onset dementia, where symptoms develop before the age of 65.

Help us raise vital funds, improve care and support for families facing dementia and spread the word about our specialist dementia nurses.

Sharing your story with Dementia UK can help to inspire and reassure others who may be going through similar things.