
“My final years with Charles shouldn’t have been as stressful as they were”
Kerry shares her experience of caring for her husband, Charles, and the difficulty finding any sort of specialist support.
Shara reflects on her journey caring for Anna, her mother, who was diagnosed with vascular dementia in 2016.

My Mum, Anna, was the strongest person I’ve ever known. She raised three daughters on her own, juggling multiple jobs, often across day and night shifts. Although this meant she couldn’t spend as much time with us as she would have liked through my teen years, she taught us how to be strong, independent and hard-working women.
Mum was at her happiest when she was cooking and feeding people. She adored having friends and family over and seeing them enjoy her food. She really was the most incredible cook. She also made and decorated wedding and celebration cakes, making all the flowers out of icing sugar. All of this was completely self-taught!
Finding outlets for her creativity was always important to Mum. We never had a garden but our balcony would become an incredible display of hanging plants and baskets, which passers-by would often stop to admire.
When she entered her mid 70s, I started to notice changes in Mum’s behaviour. Documents and paperwork were stacking up, with bills left unpaid. She had become forgetful, often leaving her food burning on the hob. And she began to withdraw socially, not wanting visitors to come around. This was completely out of character for her.
I convinced Mum to visit the GP in 2015. A year later, she was diagnosed with vascular dementia, aged 79.
I wish I could speak more positively about her post-diagnostic journey, but it has been frustrating beyond words.
It’s heartbreaking enough to hear that someone you love has just received a dementia diagnosis. But what I wasn’t expecting was the complete lack of follow-up and support afterward. I lost count of the number of health professionals who nodded their way through appointments, saying how sad it was and that it wasn’t going to get better. What we needed was a steer through what to do next, or a single point of contact, not affirmation on how tough our situation was.
When it came to social services, my frustration only compounded. Every few weeks we had a new person handling our case, meaning we had to go over the same information time and time again. And then we’d wait weeks for a decision to be made.
When I was finally successful at proving Mum had no money, was on housing credit and was in desperate need of care, they gave us access to a care team. And while I’m incredibly grateful to the carers we had, this presented so many challenges as well.
The turnover in carers was such that Mum often thought there were strangers in her own house and would become agitated. Many of them were overworked, underpaid and not adequately trained in dementia care. It got to the point where I actually ordered some leaflets and information from Dementia UK to share with the carers so they could learn more about Mum’s condition. I can certainly say that I’ve seen first-hand how woefully under-funded social care in this country really is.
I could not have coped without the Dementia UK Helpline and its dementia specialist Admiral Nurses. In the early years after Mum’s diagnosis, I felt a sense of guilt for using a service I wasn’t paying for. That sense of guilt stopped me from calling more often. Looking back, that was a mistake. Although the website has incredible advice and resources, sometimes you just need a voice, a person to speak to.
By the time I actually did call the Helpline and spoke to Admiral Nurse Kerry, I was beyond caring about my guilt. I was desperate. My advice to anyone who finds themself in this position is don’t let yourself get desperate. Use the resources as and when you need them.
Kerry was a godsend. We met regularly via virtual appointments after that initial call. In 2023, Mum suffered a number of falls, and after a traumatic 32-hour wait in A&E, she was in hospital for eight weeks. Kerry understood the pressures of the hospital setting, and suggested making a ‘patient passport’ to help care staff understand Mum’s history, her likes and dislikes and who she was as a person.
Kerry also taught me so much about Mum’s advancing frailty, and corresponding continence issues, weight loss, unmanaged pain, poor mobility and risk of falls. She guided us through the hospital discharge process and helped us find a suitable care home for Mum’s final months.
Alongside all of this, Kerry was there for me. I was so consumed with stress and worry that my own wellbeing had well and truly taken a backseat. She reminded me that in order to be the best carer I could be, I needed to look after myself too.
Mum died in April 2024. I’m still processing her loss, and grief has very much been a journey for me. But when I remember Mum, I like to think of her laughing. She had the most beautiful laugh and a smile that could light up a room. She never lost either right up to the end.

Kerry shares her experience of caring for her husband, Charles, and the difficulty finding any sort of specialist support.

When Elliott’s father was diagnosed with young onset Alzheimer’s disease in his fifties, family life was changed forever.
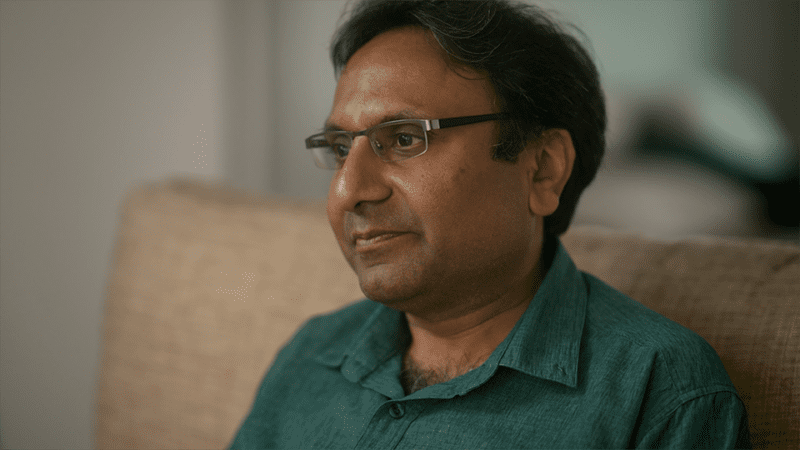
Mahersh opens up on the struggles he and wife Nishma have faced in their attempts to secure CHC funding for his mother’s care.