
“My final years with Charles shouldn’t have been as stressful as they were”
Kerry shares her experience of caring for her husband, Charles, and the difficulty finding any sort of specialist support.
Helen shares her family’s experiences of trying to navigate the fragmented health and social care system after her mum was diagnosed with Alzheimer’s disease.

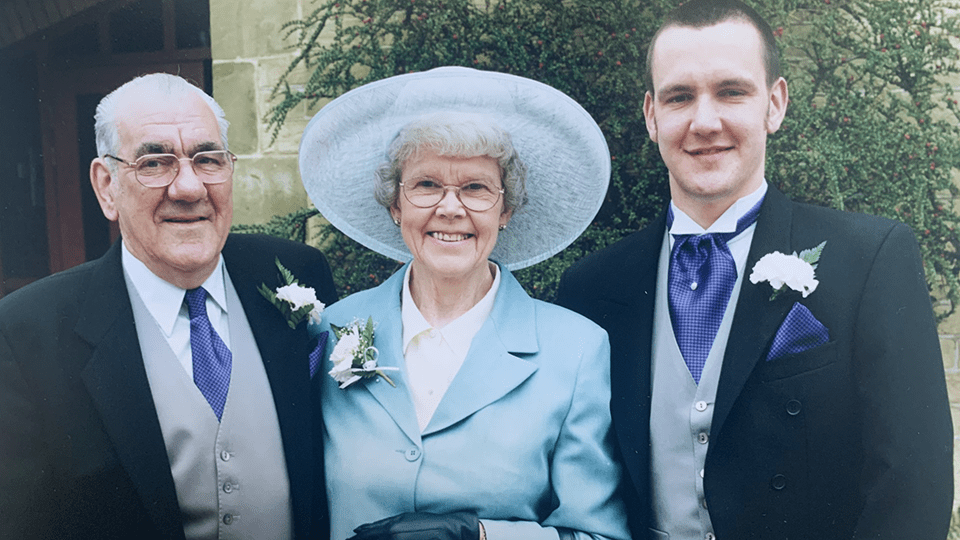
Before Alzheimer’s arrived, my mum, Maria, was as vibrant as can be. She was such a character – always friendly and smiling. Everybody loved her.
Keeping active was always very important to Mum. Her favourite way to keep active was sequence dancing; she’d do it every night if she could. So when she started wanting to go less, my two sisters and I knew something wasn’t right. We certainly didn’t suspect dementia, but looking back, that was the first sign.
In the years that followed, Mum became forgetful. She’d get cross with me for odd reasons. And she wanted to see other people less and less, which was totally unlike her.
I found it incredibly difficult to tell Mum that we thought she should see a doctor. Independence was so important to her. When she was 80, she even built a patio by herself: that’s the sort of woman she was. The thought of seeing a doctor and being told she could no longer do things was simply not something she was open to.
But we did finally convince her to go, and a few months later, she was diagnosed with Alzheimer’s disease. She was 87 years old.
I was astounded at the lack of post-diagnostic care. There was no follow-up, no signposting to other medical professionals and not even a real explanation of the condition. If I’m honest, I don’t think many of the medical professionals we’ve seen over the years have a thorough understanding of dementia.
It was left to me and my sisters to support Mum as best we could.
 In 2021, Mum, now 94 years old, had a nasty fall and had to go to hospital. Being in the midst of Covid, we weren’t allowed to visit her. We could only go off what the nurses were telling us, and they were explaining that her dementia had progressed rapidly over the course of a week. She didn’t know where she was or who all these strangers were. She must have thought we had abandoned her, which breaks my heart.
In 2021, Mum, now 94 years old, had a nasty fall and had to go to hospital. Being in the midst of Covid, we weren’t allowed to visit her. We could only go off what the nurses were telling us, and they were explaining that her dementia had progressed rapidly over the course of a week. She didn’t know where she was or who all these strangers were. She must have thought we had abandoned her, which breaks my heart.
Despite my sisters and I having lasting power of attorney, which should have enabled us to be involved in decisions about Mum’s care, a social worker talked to Mum for a few minutes at the hospital, then called us and said she could go home but needed four care visits a day. At no point were we consulted about this decision. When I asked the social worker when she’d be coming to assess Mum’s home, I was told that they didn’t do that anymore. I’m not sure how they thought they could assess Mum’s safety without even visiting her home.
But the worst was yet to come. Before Mum was discharged from hospital, the care package they’d planned fell through, so the social worker told me she was sending Mum to a care home as a temporary solution. I told her that we’d much rather care for Mum in her own home until this was sorted out. But against our wishes, Mum was put in a care home, where she stayed for nine days. On the day she arrived, I went to see her and while we were sitting together, she turned to me and said, “Am I going to be here for the rest of my life?”
It wasn’t until years later that I learned we’d had a legal right to take Mum back to her family home that day.
Mum was eventually allowed back to her own home, as long as we agreed to the four visits from carers each day. Reluctantly, I agreed. I thought between my siblings and I, we could deliver better care than what was being prescribed to us. Mum was so glad to be back in her own environment. Although the fall had caused her to lose confidence, Mum was still quite active at the time, and would relish her daily walk.
The carer visits proved more a hindrance than a help, as I suspected they would. For one, we never knew when they’d be coming and going so there was a lot of sitting around, waiting for them. Mum asked me at one point if I could get these strangers out of her house, as she felt trapped.
Eventually I got them to agree to reduce to two visits a day. Mum would’ve cancelled them altogether but I was worried that if we did that, then when she really needed help we’d never get it again.
In December 2023, I noticed Mum’s condition was deteriorating. I phoned her GP and asked if he could do a home visit as well as an assessment for continuing healthcare funding (CHC) to help with the cost of her care. We were at a stage where we could really have used the extra support. Up until this point, we were self-funding her care.
He came and took Mum’s blood pressure, which was higher than normal but still within a safe range, according to him. That was the only test he did, before advising us not to apply for CHC because if we applied too soon, we might not get it.
Of my own volition, I sought out the initial assessment form for CHC. I couldn’t believe how difficult they had made it for someone with dementia to get the funding. The wording is so confusing and gives you almost no hope that you’re eligible. The fact is, dementia in all its forms is a life-limiting disease. To deny someone the help they need because someone somewhere thinks you aren’t ill enough to be eligible is so cruel in my opinion.
Mum died the following February. As per the GP’s advice, we hadn’t even started the CHC application.

I am so sick of hearing politicians boasting about how many billions they have put into health and social care. It might as well be pennies unless they start to plan for longer than each electoral term.
It is so important that we see equal access to services, and I just hope that those who have the power to influence change in this area, do so. There is a lot of talk about fixing the NHS. In order to do this the Government must include in their review, as a priority, how to speed up the diagnosis of dementia. Equally as important is improving the care provided for dementia patients and the correct support of the loved ones that care for them. If there was a proper pathway to treatment for patients and support for carers, there would be less pressure on the NHS. Too often dementia is seen as a social care problem but it is a life limiting illness that deserves the same effort that is put into treating other serious conditions such as cancer.
As my family knows all too well, the system is simply not fit for purpose in this country when it comes to dementia.
We know that dementia care can be fixed. Join us and urge the new Government to transform dementia care so that everyone affected by dementia gets the specialist support they need. Find out more here.

Kerry shares her experience of caring for her husband, Charles, and the difficulty finding any sort of specialist support.
Over the span of a decade, Chris cared for both parents with dementia. He shares his story to highlight the systemic flaws carers face.

We need the Government to urgently review the continuing healthcare funding process so that more people with dementia can access the support.